Prior authorization is having a moment. Are you?
Recent events have made prior authorization part of the national conversation. Let’s add facts to the discussion.
Sep 4, 2025
Sep 4, 2025

Unless you’ve been totally off the grid this summer, you no doubt have noticed that prior authorization has been in the headlines. Not just in the healthcare trade press but in the mainstream media. Largely limited to an ongoing debate within healthcare, PA is now part of the national conversation.
Like all national conversations, the line between truth and untruth when it comes to PA can be fuzzy at times. So, we’re going to review a few events that have pushed PA into the spotlight and then follow up with a few facts about PA to steer the national conversation in an honest direction.
Part of that national conversation will be taking place, albeit privately, during the fall Kodiak Revenue Circle event. We’re hosting this members-only event for Kodiak Platform users at the Grand Bohemian Charleston in Charleston, South Carolina, Nov. 9-11. For more information, click here.
What got tongues wagging over PA? In chronological order, here’s what happened if you haven’t checked email, watched the news, or scrolled through your social media channels in recent days.
Insurers make a promise
On June 23, U.S. Department of Health and Human Services and Centers for Medicare & Medicaid Services officials announced that most of the nation’s commercial health insurance companies made a voluntary pledge to “fix (the) broken prior authorization system.” Their promise to “streamline and improve the prior authorization process” applies to all Medicare Advantage plans, Health Insurance Marketplace plans, Medicaid managed care plans, and commercial health plans. Specifically, the insurers vowed to do six things:
- Standardize electronic PA
- Reduce the scope of claims subject to PA
- Ensure continuity of care when patients change plans
- Enhance communication and transparency on PA determinations
- Expand real-time PA responses
- Ensure medical review of rejected PA requests
AHIP, the health insurance trade association, endorsed the voluntary pledge, saying it would benefit 257 million people enrolled in health plans covered by the insurers’ promise.
PA pilot for traditional Medicare
Four days later, on June 27, CMS announced the launch of a pilot program to test a new PA process for traditional Medicare. CMS dubbed the pilot program the Wasteful and Inappropriate Service Reduction Model, or the WISeR Model.
The WISeR Model will test the viability of using technology, including artificial intelligence, to “expedite the prior authorization processes for select items and services that have been identified as particularly vulnerable to fraud, waste, and abuse, or inappropriate use,” CMS said.
Among those vulnerable items and services are skin and tissue substitutes, electrical nerve stimulator implants, and arthroscopic knee surgery for osteoarthritis. CMS said the WISeR Model doesn’t apply to inpatient-only services, emergency services, and services that “would pose a substantial risk to patients if significantly delayed.”
The six-year pilot will run from Jan. 1, 2026, through Dec. 31, 2031.
Companies with “expertise managing the prior authorization process for other payers using enhanced technology like AI” can apply to become WISeR contractors. CMS will pay WISeR contractors on a contingency basis.
“For each selected service, participants will receive a percentage of the reduction in savings that can be attributed to their reduction of wasteful or inappropriate care,” CMS said.
Consumers are wary
On July 25, the Kaiser Family Foundation released the results of a KFF Health Tracking Poll on PA. KFF surveyed a representative sample of about 1,300 U.S. adults, asking them what they thought about PA. Here’s what the respondents told KFF:
- 73% said they think delays and denials of healthcare services by health insurance companies are a major problem.
- 51% said their health plan required them to get PA approval before they received a healthcare treatment or service within the past two years.
- 47% said getting PA approval from their health plan was “somewhat” or “very” difficult.
- 29% said their health plan delayed or denied needed care, treatment, or medication within the past two years.
Interestingly, 61% said it was “not too likely” or “not at all likely” that health insurance companies will follow through on their pledge to streamline and improve the PA process.
What the numbers say
We know what insurers are saying about PA. We know what CMS is saying about PA. And we know what consumers are saying about PA.
But what are the numbers saying about PA? Actual numbers that are not generated by special interests or in support of one position or initiative or the other.
We decided to look at three revenue cycle key performance indicators calculated from the actual data from 2,100 hospitals and 300,000 physicians that use the Kodiak Platform and Kodiak Revenue Cycle Analytics to manage their net revenue and monitor their revenue cycle performance.
The three KPIs are initial denial rate, initial denial rate caused by PA or precertification issues, and initial denial rate caused by a request for information from a payor. Collectively, the three KPIs capture what’s happening in the real world of the healthcare revenue cycle. We compared the KPIs in 2024 with the KPIs from the first six months of 2025.
This chart reveals what we found:
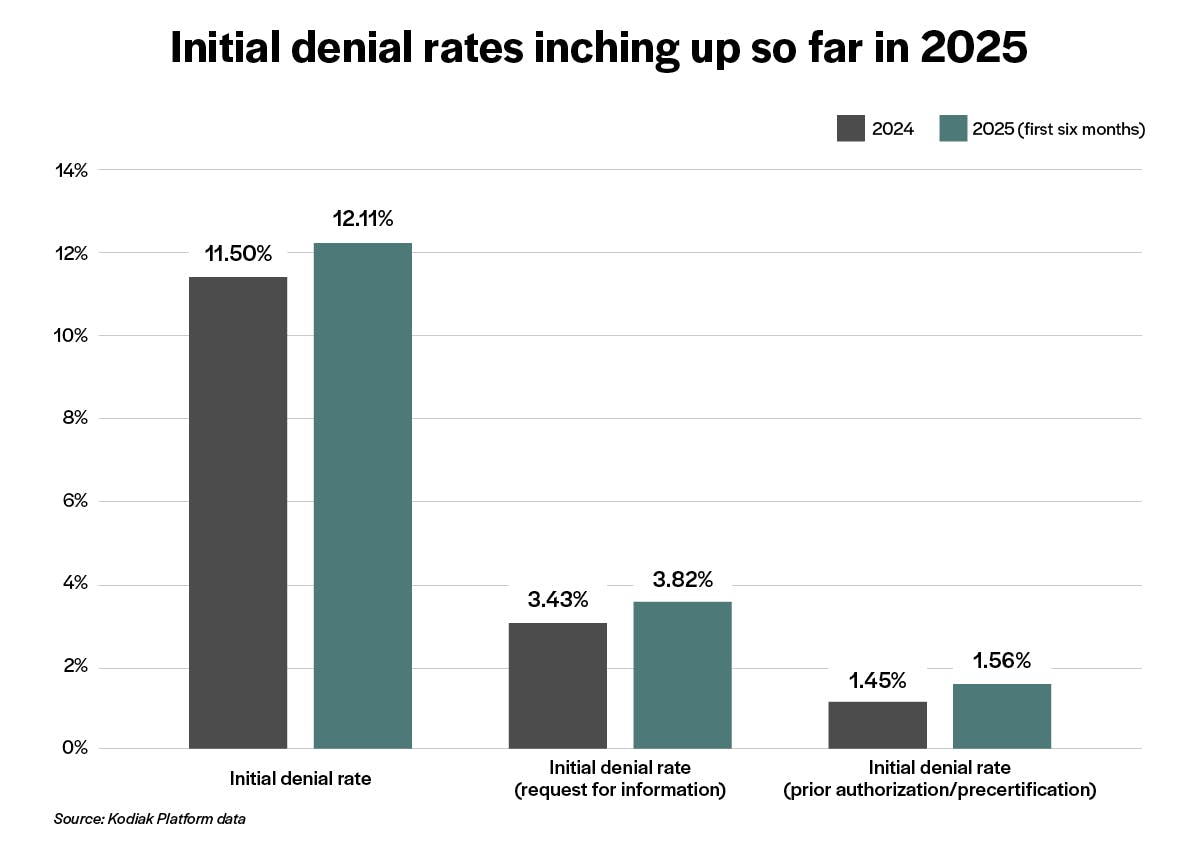
In all three cases, the KPI has crept up through the first half of this year. That suggests to us that the PA landscape is getting tougher, not easier, for providers.
We’ll be watching to see what happens to those numbers the rest of the year and into 2026 and beyond as all these new pledges and pilots roll out.
We’re certainly going to be talking about them at this year’s Revenue Circle event, whether they fall out of the national conversation about PA or not. Please watch for more pre- and post-event content from the fall Revenue Circle.
Learn more about the 2025 Fall Revenue Circle.
Want the latest updates from Kodiak?
Get access to our communications, including our Healthcare Connection newsletter, to tap into industry trends, CPE webinars, and more.


